If you have never seen the 1960s blockbuster old western, The Magnificent Seven, you may want to have a look. The movie is popular in Russia even today. Yes, the lead star, Yul Brynner was Russian, but the story itself carries several messages about values and priorities. These messages may resonate with clinicians and administrators.
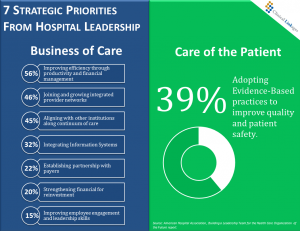
Like the Seven in the movie who chose to take on a battle for the struggling farmers of a Mexican village, hospital leaders today are developing survival tactics to deal with a very aggressive healthcare marketplace. The top 7 strategic priorities from the C-Suite are outlined in the recent report, “Building a Leadership Team for the Health Care Organization of the Future”, from the American Hospital Association
Margins Matter
The importance of financial management should not be understated. Without good stewardship there will be no hospital bed for Aunt Sue, or perhaps for readers of this post. That said, it is interesting that 6 out of the 7 top priorities of this new AHA report are business based, either directly related to the budget, or to strategies that will enhance the bottom line.
Only one strategy can be defined as directly related to patients. 39% of the respondents say adopting evidence-based practice for improvement in care quality and safety is a priority.
This chart provides a summary of the responses from more than a thousand hospital leaders. We see that improving efficiency through productivity and financial management carries the top slot, with 56% of leaders saying this is a priority. Joining provider networks and aligning with other institutions for care continuum have 46% and 45%, respectively. Integrating information systems (32%), partnership with payers (22%), strengthening finances for reinvestment/innovation (20%), and improving employee and physician engagement and leadership skills (15%) round out the rest of the survey results
Improving productivity is essential to remove waste in time and resources and a Lean approach is often used to reach the target goals. It is a tool that is also useful in removing of barriers to evidence-based practice.
Lean Evidence?
When Yul Brynner and his 6 diverse sidekicks road into the town to save the villagers from the marauding bandits, it can be said that they had a singular focus on best outcomes. It was a Lean operation, as they had only their skills and quick thinking to confront the challenge and there was very little cash as compensation.
Lean is an essential tool for improving productivity. Clinical care has many areas where Lean could free up clinicians’ time for more direct time with patients. Nurses for example spend considerable time, up to 35% of the day, documenting various aspects of patient care. A state of Maryland study showed 81% percent of nurses surveyed say documentation keeps them from direct care of patients. The challenge rests not just in streamlining processes, but in how we integrate best evidence recommendations 24/7 in care units. Will Lean alone work?
Our lag time for adopting evidence into care of patients remains woefully long; 17 years on average according to the original Institute of Medicine statistic. Current CDC data on infections reminds us that some things will take more than improved productivity to achieve optimum outcomes.
Evidence based care needs to be an expectation not an option. This may be a tough sell in today’s market because evidence translation efforts are fraught with barriers from infrastructure as well as clinician behavior. Embedding evidence 24/7 requires commitment with a vision and the support to remove barriers so clinicians can succeed and patients can benefit.
Work Environment Matters
Aunt Sue is 82 years old, hard of hearing, is a Type 1 diabetic with hypertension and in your hospital for surgery to remove a tumor in her stomach. Her peripheral circulation is not the best, despite a HgA1c of 6, and she is very frightened. Her neighbor died of cancer a month ago and you are her closest relative. What do you expect clinical staff to do to make your aunt’s situation the best it can be?
Of course they will manage her post-operative pain and keep her blood sugars in range but what is happening to help her prevent a pressure ulcer? She is already at risk for quick breakdown of her fragile skin. How long will her urinary catheter remain in the bladder? You’ve read that <48 hours is best unless there are extenuating clinical reasons, and you do not want her to get an infection.
The list can go on with someone like Aunt Sue. So how do we bridge the gap to evidence based care when time is clinicians’ most precious resource?
We have some great research on work environment as the fundamental driver of how clinicians practice. This is where Lean can help to eliminate time wasters for the clinical team. They can spend time with Aunt Sue, take her foley catheter out and see that she is taken to the bathroom frequently, and focus on the very tough issue of preventing skin breakdown.
If more than 440,000 patients are infected every year because we do not remove the foley in a timely manner, then we must examine why and develop a translation project around this issue. Lean can help with the barriers to evidence translation if we view the project from the clinical perspective of the patient and not simply efficiency.
Creating a blueprint for evidence integration in any clinical practice is essential for the team’s success. Ask this question, “How can we eliminate CAUTIs in our hospital?”
Lessons from The Magnificent Seven
- We need to believe in what we are doing because without complete commitment we will fail.
- The centerpiece of our plans must be the patient and family. Without that there is no engagement for best outcomes.
- Margins matter, but they must be balanced with the ability to carry out the core business…providing evidence based care to our patients.
Leave a Reply